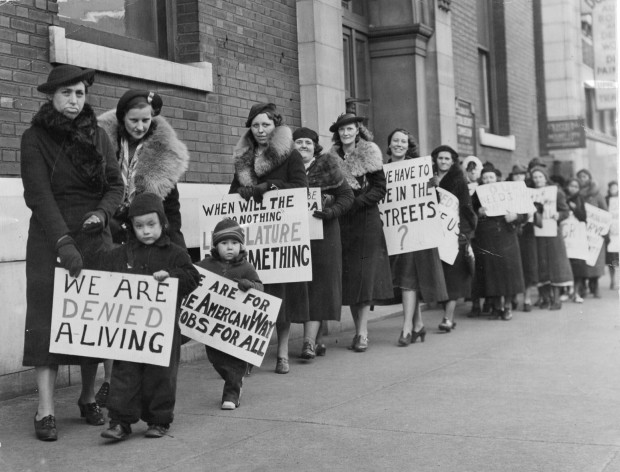
So we’re about a month into strip clubs being shut down. Before that, most in-person sex workers had already been worried about the potential of getting or spreading COVID-19 (the illness caused by the coronavirus) at work, and probably noticed a significant dip in business. Most times we’d be SOL when it comes to accessing… Continue reading Sex Workers: YOU CAN AND SHOULD REQUEST PANDEMIC RELIEF
Category: Health
Bareback: Re-Opening The Dialogue On Safer Sex In The Age of U=U
Bareback sex feels fucking amazing. I know, we’re not supposed to talk about that. We’re not supposed to talk about bareback fucking without following it up with that ubiquitous “but use a condom!” statement. However, many communities face significant barriers to condom use and have very legitimate reasons for foregoing them—and these are the communities… Continue reading Bareback: Re-Opening The Dialogue On Safer Sex In The Age of U=U
We’re Not Crazy For Doing This: Sex Workers With Mental Illness
Most people have some form of a lurid narrative about drugs, exploitation, childhood abuse, and mental illness come to mind when they imagine the life of a sex worker. However, sex workers’ relationships to their identity are far more complex and difficult to characterize than that trite narrative allows for. When it comes to sex… Continue reading We’re Not Crazy For Doing This: Sex Workers With Mental Illness
Ask Ms. Harm Reduction: Getting High With Clients
Dear Ms. Harm Reduction, I’ve been escorting and doing pro domme work for a year and a half. Sometimes I do a gram of coke with regulars, or even do drugs with new clients on occasion. I’d like to be smart about this, but I feel like I can’t ask the the sex workers I… Continue reading Ask Ms. Harm Reduction: Getting High With Clients
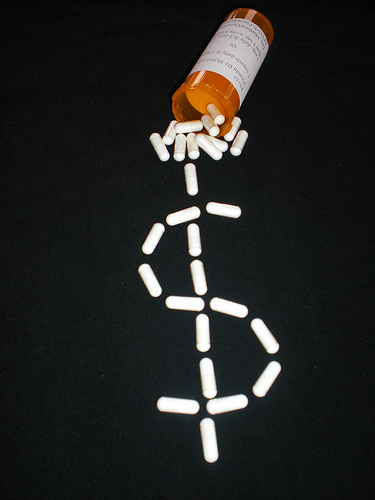
The Healthcare Hustle
Danielle is the Care Coordinator for Persist Health Project. Persist Health Project is a peer-led, community-based health and community organizing project for sex workers based in Brooklyn, New York. As Persist’s Care Coordinator, Danielle vets service providers, provides community members with supportive referrals, and helps lead Persist’s Best Practices Trainings. While many of us dream… Continue reading The Healthcare Hustle